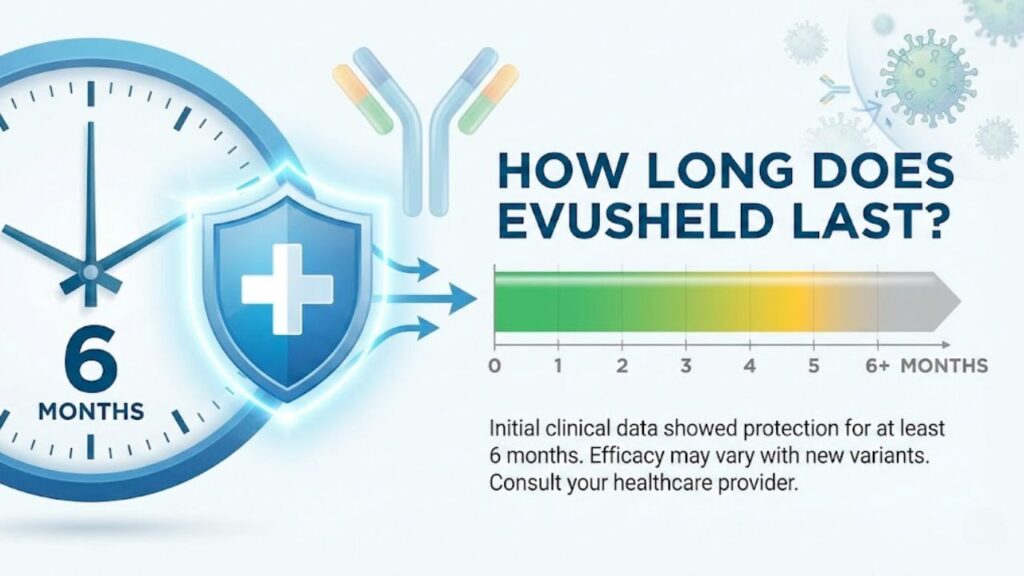
Evusheld, a groundbreaking combination of two long-acting monoclonal antibodies (tixagevimab and cilgavimab), was designed to provide extended protection against COVID-19 for immunocompromised individuals who may not respond adequately to vaccines. The duration of protection from Evusheld typically lasts approximately six months, after which repeat dosing was recommended for ongoing prophylaxis. This extended protection window made it distinct from other COVID-19 treatments, offering a safety net for vulnerable populations unable to mount sufficient immune responses through vaccination alone.
Understanding Evusheld Protection Duration
Six-Month Protection Window
Evusheld provides protection against COVID-19 for approximately six months following administration. Pharmacokinetic and pharmacodynamic modeling conducted by researchers demonstrated that drug concentrations remain effective at neutralizing certain SARS-CoV-2 variants for this six-month period after receiving the standard dose of 300mg tixagevimab and 300mg cilgavimab. The initial PROVENT clinical trial showed a relative risk reduction of 76.7 percent in symptomatic COVID-19 infection compared to placebo, with extended follow-up at a median of six months demonstrating an even higher relative risk reduction of 82.8 percent.
Repeat Dosing Schedule
For individuals requiring continuous protection, health authorities recommended repeat dosing every six months with 600mg total dose administered as two separate sequential intramuscular injections. The FDA revised the Evusheld fact sheet in June 2022 to include specific recommendations for this dosing interval based on data from a substudy of the PROVENT trial. This repeat dosing schedule was designed to maintain protective antibody levels in the bloodstream, ensuring ongoing defense against COVID-19 infection for immunocompromised patients who remained at high risk.
Initial Onset of Protection
Following administration, Evusheld begins working immediately to provide antibodies that neutralize the SARS-CoV-2 virus. Unlike vaccines that require time for the body to produce its own antibodies, Evusheld delivers pre-formed monoclonal antibodies directly into the system, offering more immediate protection for patients whose immune systems cannot effectively respond to traditional vaccination. The treatment must be observed by healthcare providers for at least one hour following injection to monitor for any potential hypersensitivity reactions.
Dosage and Administration Details
Standard Dosing Protocol
The recommended dosage of Evusheld for pre-exposure prophylaxis consists of 300mg of tixagevimab and 300mg of cilgavimab, totaling 600mg, administered as separate sequential intramuscular injections. Healthcare providers typically administer these injections in the gluteal muscles, with patients monitored for at least 60 minutes post-administration. Some health systems opted to administer four separate injections, two in each gluteal muscle, depending on concentration and formulation availability.
Preparation Requirements
Administration of Evusheld must be initiated and observed by qualified healthcare providers using aseptic technique under conditions where management of severe hypersensitivity reactions, including anaphylaxis, is possible. The medication should be brought to room temperature before injection and cannot be administered with other drugs at the same injection site. Each vial or syringe is designed for single use only, and any unused portions must be properly disposed of according to medical waste protocols.
Storage and Shelf Life
The FDA authorized an extension of the shelf-life for refrigerated lots of Evusheld from 18 months to 24 months based on stability data provided by manufacturer AstraZeneca. Proper storage conditions detailed in the authorized Fact Sheet for Health Care Providers must be strictly followed to maintain drug efficacy. Healthcare facilities were advised to retain Evusheld product appropriately even after authorization changes, in case future variants susceptible to the antibodies emerge.
Effectiveness Statistics and Clinical Data
Prevention of Severe Outcomes
A comprehensive systematic review and meta-analysis conducted by researchers from the University of Birmingham, King’s College London, and the UK Health Security Agency examined outcomes among 24,773 immunocompromised participants across 17 international studies. The analysis revealed that Evusheld demonstrated 86 percent effectiveness in preventing COVID-19-specific death, 88 percent effectiveness in preventing intensive care unit admission, and 69 percent effectiveness in preventing hospitalization. Additionally, the treatment showed 40 percent effectiveness in preventing SARS-CoV-2 infection overall among immunocompromised individuals.
Real-World Effectiveness Data
Propensity score-matched analysis of real-world data showed that Evusheld reduced the risk of symptomatic SARS-CoV-2 infection with a hazard ratio of 0.75, representing statistically significant protection compared to control groups. The incidence rate of COVID-19 hospitalization was substantially lower in the Evusheld group, with a hazard ratio of 0.41 and a number needed to treat of just 59 patients. Subgroup analyses indicated that effectiveness in reducing COVID-19 hospitalization appeared greater in non-obese patients, suggesting patient characteristics may influence treatment outcomes.
Variant-Specific Activity
Nonclinical data and pharmacokinetic modeling suggested that Evusheld retained activity against Omicron subvariants including BA.2, BA.2.12.1, BA.4, and BA.5 for six months at drug concentrations achieved following the standard 600mg dose. Studies from Oxford University and Washington University provided evidence that Evusheld maintained neutralizing activity against earlier Omicron variants like BA.1 and BA.1.1. However, the emergence of newer variants with different spike protein mutations eventually challenged the antibody’s neutralizing capacity, leading to changes in authorization status.
Current Authorization Status
United States Withdrawal
As of January 26, 2023, Evusheld is no longer authorized by the U.S. Food and Drug Administration for emergency use and became unavailable to patients. This decision stemmed from data demonstrating that Evusheld does not effectively neutralize many newer COVID-19 variants circulating in the population. The FDA revised the emergency use authorization to specify that Evusheld could only be used if more than 10 percent of circulating variants were expected to be neutralized by it, but CDC data showed that variants not neutralized by Evusheld comprised more than 90 percent of cases across all U.S. regions.
European Union Status
On September 12, 2025, the European Commission withdrew the marketing authorization for Evusheld in the European Union. The product had initially received marketing authorization on March 25, 2022, for both pre-exposure prophylaxis and treatment of COVID-19, with authorization valid for a five-year period. The withdrawal reflected evolving viral epidemiology and the reduced clinical utility of the monoclonal antibody combination against predominant circulating strains.
Product Retention Recommendations
Despite authorization withdrawal, the U.S. Government recommended that healthcare facilities and providers with Evusheld retain all product inventory in storage. This precautionary measure accounts for the possibility that SARS-CoV-2 variants susceptible to Evusheld neutralization might become more prevalent again in the future. Retained product must be stored according to specifications detailed in the authorized Fact Sheet for Health Care Providers and the Letter of Authorization.
Target Population and Eligibility
Immunocompromised Individuals
Evusheld was specifically designed for individuals with moderate to severe immune compromise who may not mount adequate immune response to COVID-19 vaccination. This included patients with primary immunodeficiency disorders, those receiving active cancer treatment, solid organ transplant recipients taking immunosuppressive medications, and individuals with advanced HIV infection. The treatment addressed a critical unmet medical need for populations who remained highly vulnerable despite widespread vaccine availability.
Vaccine Non-Responders
Some individuals with severe allergies or contraindications to COVID-19 vaccines were also considered for Evusheld prophylaxis. Additionally, patients who demonstrated poor antibody response following complete vaccination series qualified for consideration. Healthcare providers evaluated each patient’s specific medical history, concurrent medications, and risk factors to determine appropriateness for Evusheld administration.
Administration Settings
Unlike many COVID-19 treatments requiring hospital-based infusion, Evusheld could be administered in community settings, primary care offices, and outpatient clinics. This accessibility made it more convenient for immunocompromised patients to receive ongoing prophylactic protection without requiring hospitalization. However, appropriate monitoring equipment and personnel trained in managing allergic reactions had to be available at all administration sites.
Comparison with Other COVID-19 Preventions
Vaccines vs. Monoclonal Antibodies
While COVID-19 vaccines stimulate the recipient’s immune system to produce its own antibodies and cellular immunity, Evusheld provided immediate passive immunity through directly administered monoclonal antibodies. Vaccines typically require weeks to generate protective immune responses and depend on the recipient’s immune system functioning adequately. Evusheld offered an alternative for individuals whose compromised immune systems could not respond effectively to vaccination, though it did not replace vaccination when feasible.
Duration Comparison
The six-month protection duration of Evusheld significantly exceeded that of other monoclonal antibody treatments used for COVID-19, which typically provided protection lasting only weeks. This extended duration resulted from modifications to the antibody structure that prolonged their presence in the bloodstream. Vaccines generally provide longer-lasting protection through memory immune cells, but this benefit does not apply to immunocompromised individuals who cannot generate robust memory responses.
Cost and Accessibility Factors
Monoclonal antibody treatments like Evusheld represented significant healthcare investments, with production costs substantially higher than vaccines. The requirement for repeat dosing every six months added to cumulative healthcare expenditures for ongoing protection. However, for immunocompromised populations lacking alternative protective options, these treatments provided essential defense against severe COVID-19 outcomes and hospitalizations.
Side Effects and Safety Considerations
Common Adverse Reactions
Clinical trial data from the PROVENT study showed that Evusheld was generally well-tolerated among participants. Most adverse reactions were mild to moderate in severity, including injection site reactions such as pain, redness, or swelling. Systemic reactions occurred less frequently but could include headache, fatigue, and cough. Serious hypersensitivity reactions including anaphylaxis were possible but rare, necessitating the one-hour observation period post-administration.
Long-Term Safety Profile
The median duration of safety follow-up in clinical trials was approximately 84 days, with some participants followed for up to 166 days. Long-term safety data from real-world use supplemented controlled trial findings, with ongoing pharmacovigilance monitoring throughout the authorization period. Cardiac adverse events, which emerged as concerns with some other monoclonal antibody treatments, were monitored but did not show significant signals in Evusheld studies.
Drug Interactions
Evusheld could be administered regardless of concurrent medications, as monoclonal antibodies generally do not interact with conventional pharmaceuticals through metabolic pathways. However, patients receiving immunosuppressive therapies required careful monitoring, as these medications could theoretically affect antibody persistence or function. No specific drug contraindications were identified during clinical development, though comprehensive medication histories were recommended before administration.
Future Perspectives and Alternative Options
Variant-Adapted Antibodies
Research continues into next-generation monoclonal antibodies engineered to maintain neutralizing activity against diverse SARS-CoV-2 variants. Pharmaceutical developers are exploring antibody combinations targeting multiple epitopes on the spike protein to reduce susceptibility to immune escape. Future formulations may offer broader coverage and potentially longer duration of protection than first-generation products like Evusheld.
Alternative Prophylactic Strategies
For immunocompromised individuals who previously relied on Evusheld, alternative preventive strategies now include updated COVID-19 vaccines specifically formulated against current circulating variants. Additional dose series and frequent booster vaccinations may provide some protection even in immunocompromised populations, though responses remain variable. Non-pharmaceutical interventions including masking, distancing, and avoiding crowded indoor spaces continue to play important roles in risk reduction.
Antiviral Medications
Oral antiviral medications like nirmatrelvir-ritonavir and molnupiravir offer treatment options for immunocompromised individuals who develop COVID-19 infection despite prophylactic measures. These medications work through different mechanisms than antibodies and remain effective against variants resistant to monoclonal antibody treatments. Early initiation within days of symptom onset maximizes their effectiveness in preventing progression to severe disease.
Conclusion
Evusheld represented a significant advancement in COVID-19 prevention for immunocompromised populations, offering approximately six months of protection from a single administration and establishing an important precedent for long-acting antibody therapies. While the emergence of antibody-resistant variants led to withdrawal of authorization in the United States and European Union, the clinical development program provided valuable insights into passive immunization strategies and protection duration. The real-world effectiveness data demonstrated substantial reductions in hospitalizations, ICU admissions, and deaths among vulnerable patients during the period when circulating variants remained susceptible. For patients who previously benefited from Evusheld, healthcare providers now recommend updated vaccines, additional booster doses, prompt antiviral treatment when infections occur, and continued vigilance with preventive measures to minimize COVID-19 exposure risks.